
Several social media posts in Papua New Guinea claim that COVID-19 vaccines cause an immune response which makes vaccinated people sicker if they become infected.
The text of the Facebook posts (see here, here and here) is attributed to a PNG doctor, claiming “all RNA virus vaccines have failed” because of “a phenomenon called ‘immune dependent enhancement'” and that “vaccinated subjects when exposed to the same virus, subtypes and variants will become very sick and admit (sic) to hospital”.
However, there’s no evidence to support the claim. Scientists point out that COVID-19 vaccines were developed to avoid the occurrence of vaccine enhanced disease (VED), more commonly referred to as antibody dependent enhancement (ADE), and they have proven effective in reducing the risk of serious illness due to the virus.
ADE can occur when antibodies generated during an immune response to a disease actually admit the entry of the virus and its replication, leading to enhanced infection.
There is no evidence of ADE in people vaccinated for COVID-19, experts told AAP FactCheck. In addition, many studies worldwide have identified that COVID-19 vaccinations prevent severe disease and hospitalisation.
Cassandra Berry, a professor of immunology at Murdoch University in Western Australia, says ADE was discovered with some other viruses “but has not been widely found for the COVID-19 virus, SARS-CoV2 in humans”.
“(ADE) is a potential risk that was carefully considered in vaccine development,” she told AAP FactCheck in an email. “Not all viruses are the same. ADE has not been observed for a multitude of viruses.”
ADE has been a problem with some vaccines in the past including ones for dengue fever, measles and respiratory syncytial virus (RSV) – a common respiratory virus.
As early as April 2020, researchers warned of the risk of ADE in COVID-19 vaccines, noting: “In our rush to develop vaccines and antibody-based therapies, we should be mindful of what we have learned about ADE from SARS-CoV-1, HIV, and dengue virus research.”
Wen Shi Lee and Adam Wheatley, of Melbourne’s Peter Doherty Institute for Infection and Immunity, wrote an article in September 2020 for Nature Microbiology examining the possibility of COVID vaccines causing ADE. In that article, they recommended “ongoing animal and human clinical studies to provide important insights into the mechanisms of ADE in COVID-19.”
However, Dr Lee and Dr Wheatley told AAP FactCheck in May that ADE in approved COVID-19 vaccines was “very unlikely” and there was no evidence to date from the field that the phenomenon was occurring.
In a recent follow-up email, Dr Lee said this was still the case in November, adding: “I still have not seen any compelling evidence that COVID vaccines cause ADE.”
An article by experts from the Meedan Health Desk initiative notes: “In the process of making COVID-19 vaccines, scientists developed vaccine strategies around avoiding ADE”. These included animal testing and human trials, as well as “targeting a SARS-CoV-2 protein that was the least likely to cause ADE”.
Leah Katzelnick, chief of the viral epidemiology and immunity unit at the US National Institute of Allergy and Infectious Diseases, co-authored a 2020 paper, COVID-19 Vaccines: Should we fear ADE? The paper found it was “unlikely” that COVID vaccines might sensitise humans to antibody-dependent enhanced breakthrough infections.
“The point of that article is that we do not think ADE is likely to be a problem for COVID,” Dr Katzelnick told AAP FactCheck via email. “This has also been shown by the data on millions of individuals who have received the COVID vaccines.”
Multiple studies have established that vaccination reduces rates of serious illness and hospitalisation for COVID-19.
Data collected by the Centers for Disease Control and Prevention (CDC) shows the hospitalisation rate for COVID-19 treatment among US adults is about 12 times higher in the unvaccinated than the vaccinated. (see page Rates of COVID-19 Cases and Deaths by Vaccination Status)
Data from the UK analysed by Public Health England shows both the Pfizer-BioNTech and Oxford-AstraZeneca vaccines were highly effective at preventing hospitalisation with the Delta variant.
A study of US healthcare workers published in the New England Journal of Medicine found vaccine effectiveness against symptomatic COVID infection with full doses of Pfizer was 89 per cent and 96 per cent for Moderna.
The PNG doctor credited as the source of the Facebook post has been debunked previously for spreading misinformation about COVID-19. Claims that COVID vaccines can lead to ADE have also been debunked by other fact-checking organisations – see here, here, here and here.
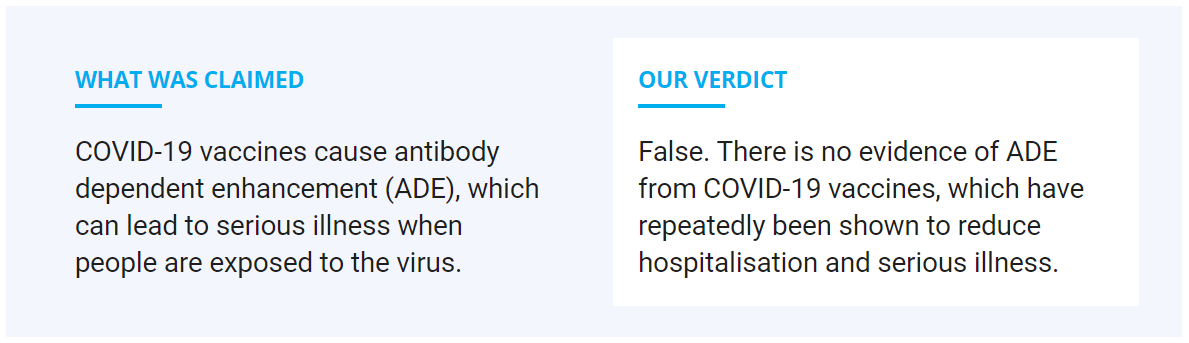
THE VERDICT
There is no evidence to indicate COVID-19 vaccines cause antibody dependent enhancement. Rather, they have been consistently shown in studies and from real-world data to reduce rates of illness and hospitalisation due to the virus.
False – The claim is inaccurate.
AAP FactCheck is an accredited member of the International Fact-Checking Network. To keep up with our latest fact checks, follow us on Facebook, Twitter and Instagram.
Story first published on AAP FactCheck
